Key Points to Understand
- Narcolepsy and insomnia are both sleep disorders but have distinct causes and symptoms.
- Narcolepsy often includes sudden sleep attacks and excessive daytime sleepiness.
- Insomnia is characterized by difficulty falling or staying asleep, leading to poor sleep quality.
- Some symptoms, like disrupted sleep, can overlap between the two conditions.
- Accurate diagnosis is crucial for effective treatment and improving quality of life.
Connection Between Narcolepsy and Insomnia
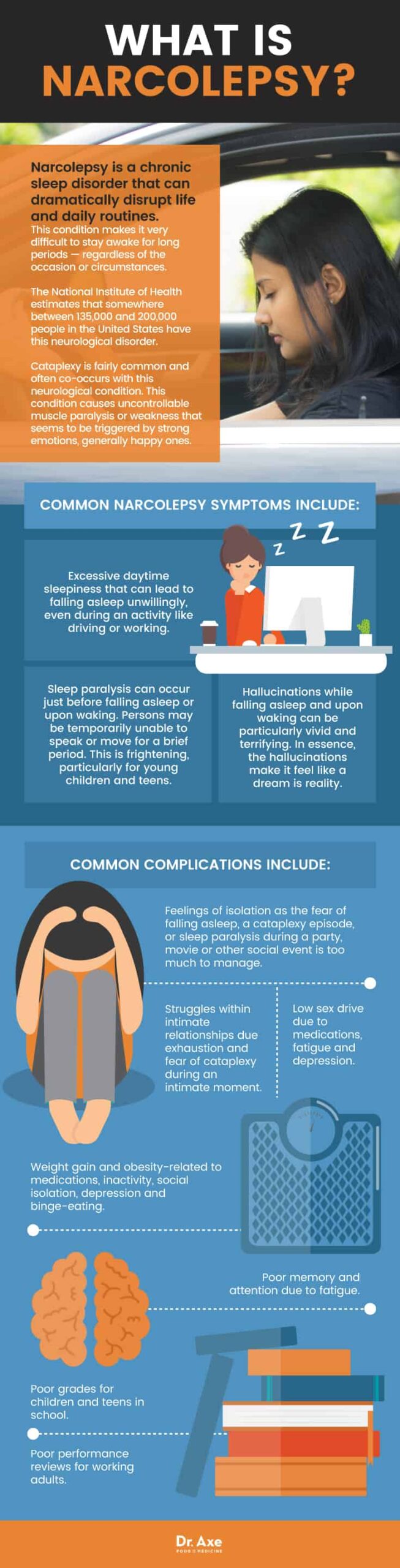
“Narcolepsy Causes & Symptoms + Natural …” from draxe.com
Exploring the Connection Between Narcolepsy and Insomnia
When we talk about sleep disorders, narcolepsy and insomnia often come up in conversation. At first glance, they seem like opposites. Narcolepsy is about falling asleep too easily, while insomnia is about not being able to sleep at all. But here’s where it gets interesting—they can sometimes be connected in unexpected ways. Understanding this connection can help us better manage these conditions and improve our sleep health.
Common Misconceptions
Many people believe that narcolepsy and insomnia cannot coexist because they appear to be opposite conditions. However, this is not entirely true. In fact, it’s possible for someone with narcolepsy to experience insomnia symptoms. This can happen because the sleep cycles in narcolepsy are often disrupted, leading to poor nighttime sleep quality, much like insomnia.
Another misconception is that both conditions are purely psychological. While stress and mental health can influence sleep, both narcolepsy and insomnia have biological and neurological components. Recognizing this helps in seeking appropriate treatment and understanding that lifestyle changes alone may not be enough.
Symptoms that Overlap
Despite their differences, narcolepsy and insomnia share some overlapping symptoms. One of the most notable is disrupted sleep. People with narcolepsy often wake up frequently during the night, similar to those with insomnia. This results in fragmented sleep, which can lead to fatigue and irritability during the day.
Another shared symptom is excessive daytime sleepiness. Although more pronounced in narcolepsy, people with insomnia may also feel tired during the day due to poor nighttime sleep. This can make daily activities challenging and affect overall quality of life.
- Frequent nighttime awakenings
- Daytime fatigue
- Difficulty concentrating
- Memory problems
Impact on Quality of Sleep
The quality of sleep is crucial for our health and well-being. Both narcolepsy and insomnia can significantly impact this quality, albeit in different ways. Narcolepsy can lead to sudden sleep attacks and disrupted sleep architecture, while insomnia results in difficulty falling asleep or staying asleep.
Most importantly, the lack of restful sleep can have cascading effects on physical and mental health. It can lead to mood disorders, increased risk of accidents, and decreased productivity. Therefore, addressing these conditions is not just about getting more sleep, but about improving the quality of that sleep.
Understanding Narcolepsy
Narcolepsy is a neurological disorder that affects the brain’s ability to regulate sleep-wake cycles. It is often misunderstood and misdiagnosed, which can delay treatment and management. Understanding its symptoms and causes is the first step towards effective intervention.
Connection Between Narcolepsy and Insomnia
One of the hallmark symptoms of narcolepsy is excessive daytime sleepiness, which can lead to sudden and uncontrollable sleep episodes. These episodes can occur at any time, often without warning. People with narcolepsy may also experience cataplexy, a sudden loss of muscle tone triggered by strong emotions.
Definition and Symptoms
Narcolepsy is characterized by several key symptoms:
- Excessive daytime sleepiness
- Cata-plexy (sudden muscle weakness)
- Sleep paralysis
- Hallucinations
These symptoms can vary in intensity and may not all be present in every individual. The sudden onset of sleep and cataplexy can be particularly disruptive, affecting daily life and safety.
Causes and Risk Factors
The exact cause of narcolepsy is not fully understood, but it is believed to be related to the loss of a neurotransmitter called hypocretin, which helps regulate wakefulness. Genetic factors may also play a role, as narcolepsy can run in families.
Besides that, certain infections, autoimmune disorders, and even head injuries have been linked to the development of narcolepsy. It’s important to recognize these risk factors as they can guide diagnosis and treatment.
Treatment Options
Treating narcolepsy often involves a combination of medication and lifestyle changes. Stimulants and antidepressants are commonly prescribed to help manage symptoms. Additionally, scheduled naps and a regular sleep routine can help improve sleep quality.
It’s essential to work closely with a healthcare provider to tailor treatment to individual needs. This personalized approach can significantly enhance quality of life and reduce the impact of symptoms.
Daily Life with Narcolepsy

“Infographic) | MyNarcolepsyTeam” from www.mynarcolepsyteam.com
Living with narcolepsy requires adjustments and coping strategies. It’s crucial to educate family, friends, and employers about the condition to foster understanding and support. Having a plan for managing sleep episodes and maintaining a consistent sleep schedule can help mitigate the effects of narcolepsy on daily activities.
Additionally, joining support groups and connecting with others who have narcolepsy can provide valuable insights and encouragement. Remember, you are not alone, and with the right support and management, it is possible to lead a fulfilling life.
Understanding Insomnia
Insomnia is one of the most common sleep disorders, characterized by difficulty falling or staying asleep. It can be acute, lasting a few days or weeks, or chronic, persisting for months or even years. Understanding the underlying causes and symptoms is crucial for effective treatment.
Insomnia can have many triggers, including stress, anxiety, depression, and lifestyle factors. Identifying and addressing these triggers is often the first step in managing the condition.
Symptoms of insomnia include:
- Difficulty falling asleep
- Frequent nighttime awakenings
- Waking up too early
- Daytime fatigue and irritability
These symptoms can vary in severity and may fluctuate over time. Recognizing them early can help prevent chronic insomnia and its associated health risks.
Differences Between Narcolepsy and Insomnia
While narcolepsy and insomnia are both sleep disorders, they have distinct differences in their causes, symptoms, and impacts on daily life. Understanding these differences is crucial for accurate diagnosis and treatment.
Diagnosis Criteria
The diagnosis of narcolepsy typically involves a combination of medical history, sleep studies, and sometimes a multiple sleep latency test (MSLT). This test measures how quickly a person falls asleep in a quiet environment during the day and whether they enter REM sleep quickly, which is indicative of narcolepsy.
Insomnia diagnosis, on the other hand, often relies on patient-reported sleep diaries, questionnaires, and sometimes actigraphy, which measures movement to estimate sleep patterns. The focus is on identifying patterns of sleep disruption and any contributing factors.
- Narcolepsy diagnosis often involves sleep studies and MSLT.
- Insomnia diagnosis relies on sleep diaries and questionnaires.
- Both conditions require a thorough evaluation of sleep habits and health history.
Effects on Daily Functioning
Narcolepsy and insomnia both significantly affect daily functioning, but in different ways. Narcolepsy often leads to excessive daytime sleepiness, which can result in sudden sleep attacks and difficulty maintaining alertness. This can impact work, school, and social interactions.
Insomnia, by contrast, typically results in fatigue, irritability, and difficulty concentrating during the day. The chronic lack of restorative sleep can lead to mood disturbances and decreased cognitive function, affecting performance in various aspects of life.
Variations in Treatment Approaches
Treatment approaches for narcolepsy and insomnia differ due to the nature of each condition. Narcolepsy treatment often involves medications such as stimulants to promote wakefulness and antidepressants to manage cataplexy. Lifestyle adjustments, including scheduled naps and sleep hygiene, are also important.
Insomnia treatment, as mentioned earlier, focuses on behavioral therapies like CBT-I and lifestyle modifications. Medications may be used for short-term relief, but the emphasis is on creating sustainable sleep habits to improve long-term sleep quality.
Research on the Co-Occurrence of Narcolepsy and Insomnia
Recent research has explored the intriguing co-occurrence of narcolepsy and insomnia. Although they are distinct disorders, they can overlap, leading to complex cases that require nuanced treatment approaches. Understanding this overlap is crucial for developing effective management strategies.
Studies suggest that disrupted sleep architecture in narcolepsy can mimic insomnia symptoms, such as frequent awakenings and difficulty maintaining sleep. This overlap can complicate diagnosis and treatment, highlighting the need for comprehensive sleep evaluations.
One study found that 37% of narcolepsy patients reported insomnia-like symptoms, indicating a significant overlap between these conditions.
This finding underscores the importance of considering both conditions when evaluating sleep disorders and tailoring treatment plans to address the unique challenges of each individual.
Notable Case Studies
- Case Study 1: A 25-year-old woman diagnosed with narcolepsy experienced insomnia-like symptoms, leading to a revised treatment plan that incorporated CBT-I techniques.
- Case Study 2: A 40-year-old man with chronic insomnia was later diagnosed with narcolepsy, highlighting the importance of comprehensive sleep assessments.
These case studies illustrate the complexity of diagnosing and treating co-occurring sleep disorders. They emphasize the need for personalized treatment approaches that consider the full spectrum of symptoms and their impact on daily life.
In conclusion, understanding the connection between narcolepsy and insomnia is essential for accurate diagnosis and effective treatment. By recognizing the unique characteristics and overlaps of these conditions, we can develop more targeted interventions that improve sleep quality and overall well-being.
Future Implications for Treatment
As we continue to unravel the complexities of sleep disorders like narcolepsy and insomnia, future treatments may become more targeted and effective. Advances in genetic research and neuroimaging are shedding light on the underlying mechanisms of these conditions, paving the way for innovative therapies.
- Development of new medications that specifically target sleep-wake regulation.
- Personalized treatment plans based on genetic and neurobiological profiles.
- Integration of technology, such as wearable sleep monitors, to enhance diagnosis and treatment.
These advancements hold promise for improving the quality of life for those affected by sleep disorders. By focusing on the root causes and individual variations, we can move towards more precise and effective treatments.
Moreover, public awareness and education about sleep disorders are crucial. Understanding the impact of sleep on overall health can encourage early diagnosis and intervention, ultimately leading to better outcomes for individuals with narcolepsy, insomnia, or both.
Key Takeaways and Moving Forward
In summary, while narcolepsy and insomnia are distinct sleep disorders, they share some overlapping symptoms and challenges. Accurate diagnosis and tailored treatment are essential for managing these conditions effectively.
Summary of Key Differences and Links
Narcolepsy is primarily characterized by excessive daytime sleepiness and sudden sleep attacks, while insomnia involves difficulty falling or staying asleep. Despite these differences, both conditions can disrupt sleep quality and daily functioning.
Understanding the potential overlap and co-occurrence of symptoms is crucial for effective treatment. By recognizing these connections, healthcare providers can develop comprehensive management strategies that address the unique needs of each individual.
Emphasizing Accurate Diagnosis
Accurate diagnosis is the cornerstone of effective treatment for sleep disorders. A thorough evaluation, including sleep studies and patient history, is essential for identifying the underlying causes and tailoring treatment plans accordingly.
Recommendations for Patients
For those living with narcolepsy, insomnia, or both, it’s important to work closely with healthcare providers to develop a personalized treatment plan. Prioritizing good sleep hygiene, adhering to prescribed medications, and considering behavioral therapies can help improve sleep quality and overall well-being.
Future Directions in Research
Ongoing research is exploring the genetic, neurobiological, and environmental factors contributing to sleep disorders. These studies aim to uncover new treatment options and improve existing therapies, ultimately enhancing the lives of those affected by narcolepsy and insomnia.
As we continue to learn more about these complex conditions, collaboration between researchers, clinicians, and patients will be key to advancing our understanding and improving treatment outcomes.
Frequently Asked Questions (FAQ)
Here are some common questions about narcolepsy and insomnia to help clarify these conditions and their management.
What is the main difference between narcolepsy and insomnia?
The main difference lies in the symptoms and causes. Narcolepsy is characterized by excessive daytime sleepiness and sudden sleep attacks due to disrupted sleep-wake regulation. Insomnia involves difficulty falling or staying asleep, often linked to stress, anxiety, or lifestyle factors.
Can a person have both narcolepsy and insomnia?
Yes, it’s possible for someone to experience symptoms of both narcolepsy and insomnia. Disrupted sleep in narcolepsy can mimic insomnia symptoms, leading to a complex interplay between the two conditions.
How can someone manage symptoms of both conditions simultaneously?
Managing both narcolepsy and insomnia requires a comprehensive approach. This includes working with healthcare providers to develop a tailored treatment plan, incorporating medication, behavioral therapies, and lifestyle changes. Prioritizing good sleep hygiene and addressing any underlying health issues can also help improve sleep quality.
